Sickle cell disease (SCD) affects around 100,000 Americans and presents numerous health-related challenges thus necessitating effective management strategies. Educational initiatives on evidence-based intervention are known to play a crucial role in improving patient-related outcomes (PRO) and enhancing the quality of life (QOL) for individuals with SCD.
Community-based hospitals face challenges in managing SCD patients. Patients who are unaffiliated with a comprehensive sickle cell center have increased healthcare utilization, readmissions, and patient dissatisfaction due to limited access to specialized services and discrepancies in care delivery. Addressing these disparities and expanding access to care is crucial in optimizing SCD management.
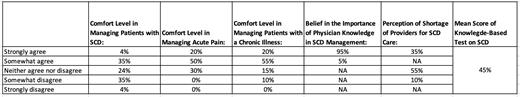
The purpose of this exploratory observational study was to identify provider-related gaps in a community-based tertiary center. The survey assessed internal medicine trainees' and hospitalists' baseline knowledge and comfort level at a tertiary care center with a total of 304 yearly adult admissions related to SCD management. The survey was distributed through an online platform. Data was analyzed to identify trends and gaps in internal medicine providers. Our survey had a total of 30 respondents, the response rate was 39%. Most respondents (90%) had prior experience with SCD patients; however, many gaps were identified [Table 1]. 70-75% of physicians felt comfortable managing acute pain and chronic illnesses, yet only half of these providers were comfortable with managing SCD patients.
While our study sample is small, similar results were noted in a study conducted in another community-based hospital in the Chicagoland area. Our study shows a similar provider-related gap in SCD care delivery. Dr. Kanter proposed a model of care delivery which is known as the “hub and spoke” model. It offers a promising solution, creating a networked system of care with a central hub and secondary spokes providing more limited services. Community-based hospital settings can serve as spokes, bringing specialized SCD care closer to patients in local areas. Hence, we propose that this model can be further modified to include provider education. This equips non-sickle cell specialists at various spokes with the necessary knowledge and skills through targeted education by sickle cell specialists at a centralized hub. Targeting provider gaps may significantly improve PRO. Our residency program hopes to establish an affiliation with the University of Illinois (UI) Health Sickle Cell Center (SCC) to help with educating trainees on SCD. The UI Health SCC was one of eight sites participating in the National Sickle Cell Disease Implementation Consortium (SCDIC) with the goal of helping patients access longitudinal care, increase hydroxyurea utilization when appropriate, and provide proper pain management in ED. They are also part of the Recruitment and Engagement in Care to Impact Practice Enhancement (RECIPE) project which focuses on patients with SCD that are unaffiliated with care centers and attempts to understand and eliminate their barriers to care. Future efforts should include implementing targeted provider education, within the context of a hub and spoke model. This may help bridge the gap in care delivery and ultimately enhance outcomes for SCD patients.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal